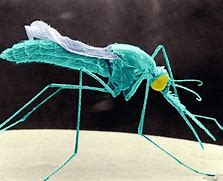
Compelling evidence has emerged that a malaria outbreak in Ethiopia this year was caused by the arrival in eastern Africa of an insecticide-resistant species of mosquito (Anopheles stephensi).
The finding complicates disease-elimination efforts in Africa – where 95 per cent of the world’s malaria infections occur – and has worried researchers because A. stephensi’s behaviour is different from that of other malaria carriers.
Outbreaks have been difficult to control in Africa recently because healthcare workers and researchers have been focused on the Covid-19 pandemic. From 2019 to 2020, malaria infections in Africa rose by seven per cent, to about 228 million.
Researchers have been warning that A. stephensi, which is prevalent in southern Asia, could be behind recent malaria surges in eastern Africa. And data presented on November 1 at the annual meeting of the American Society of Tropical Medicine and Hygiene point strongly to the mosquito species being the culprit in the outbreak in Dire Dawa, Ethiopia.
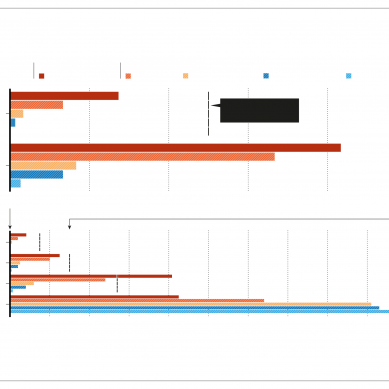
“This is very important work,” says Seth Irish, a medical entomologist at the World Health Organization (WHO) in Geneva, Switzerland. The data are especially convincing, says Jaishree Raman, a molecular biologist at the National Institute for Communicable Diseases in Johannesburg, South Africa, because before A. stephensi arrived, malaria infections had not been common in Dire Dawa. But cases have skyrocketed, from 205 in 2019 to more than 2,400 so far in 2022.
To determine whether A. stephensi is indeed driving the malaria surge in Dire Dawa, Fitsum Tadesse, a molecular biologist at the Armauer Hansen Research Institute in Addis Ababa, Ethiopia, and his colleagues identified 98 residents who had tested positive for the disease.
They then tested 213 people who shared a household with those residents, as well as 213 people living with a person who had tested negative. Those in the first group were about four times more likely to also have the disease.
The results suggest that a mosquito, which can pick up malaria parasites from the blood of an infected person and spread them to others nearby, is involved in the outbreak. To pinpoint the exact species, the researchers looked for breeding sites and collected adult mosquitoes from around the homes of those included in the study. About 97 per cent of the adult mosquitoes collected were A. stephensi and researchers found more breeding sites around the households of those who had tested positive for malaria.
One reason that scientists have been worried about A. stephensi is that it is adept at breeding in human-made water containers, such as barrels or wells, making urban areas a preferred spot. By contrast, other malaria-carrying mosquitoes often prefer to breed in stagnant puddles and lakes in rural settings.
Many African cities are rapidly urbanising, offering ample opportunities for A. stephensi to find suitable breeding grounds, Irish says. And its larvae are especially resilient, Tadesse says; the mosquito persists even during dry seasons, unlike other malaria carriers, which die off without adequate breeding sites.
Another concern is that A. stephensi prefers outdoor settings to indoor ones, rendering some conventional methods of mosquito control, such as bed nets and household spraying, ineffective. It’s “questionable how feasible malaria elimination is with existing tools”, says Jan Kolaczinski, who leads the vector control and insecticide resistance unit at the WHO’s Global Malaria Programme.
Given that A. stephensi is also resistant to common insecticides, such as DDT and pyrethroids, Kolaczinski stresses the importance of thinking outside the box to stop the insect’s spread. He recommends more research into the use of genetically modified mosquitoes to prevent A. stephensi from breeding, for example.
Lessons from treating A. stephensi in India, where the mosquito has caused urban malaria outbreaks, could also help, says Pradeep Srivastava, a former chief of vector control and entomology at the National Center for Vector Borne Diseases Control in Delhi. One strategy that has worked is enacting stricter policies on water storage, he says.
The stakes are high: Djibouti, which neighbours Ethiopia, was on the verge of eliminating malaria from its borders in 2012, when researchers there first encountered A. stephensi. Since then, infections have ballooned, with more than 73,000 reported in 2020.
In recent years, the mosquito species has been observed in northern Nigeria, thousands of kilometres across the continent. The WHO issued an alert about A. stephensi in 2019, and this September the agency launched an initiative to stop its spread.
A 2020 analysis also found that about 126 million people living in African cities could be at risk of malaria if A. stephensi continues to spread across the continent. The WHO is coordinating a pilot programme to distribute a malaria vaccine that was approved in 2021 for broad use in children.
The vaccine, which works by creating antibodies against the deadliest species of malaria parasite (Plasmodium falciparum), will have limited release in Kenya, Malawi and Ghana, and will be available in other malaria-endemic countries by 2025.
“There is no silver bullet” for this fast-spreading malaria vector, Tadesse says. “We need a different approach.”
- A Nature report