There could be an even more effective drug in town for weight management – namely tirzepatide.
As the world struggles with obesity ‘epidemic’ tirzepatide has emerged has emerged as one of the newest antidotes to a problem that is ravaging the younger population as a result of rapidly changing lifestyles.
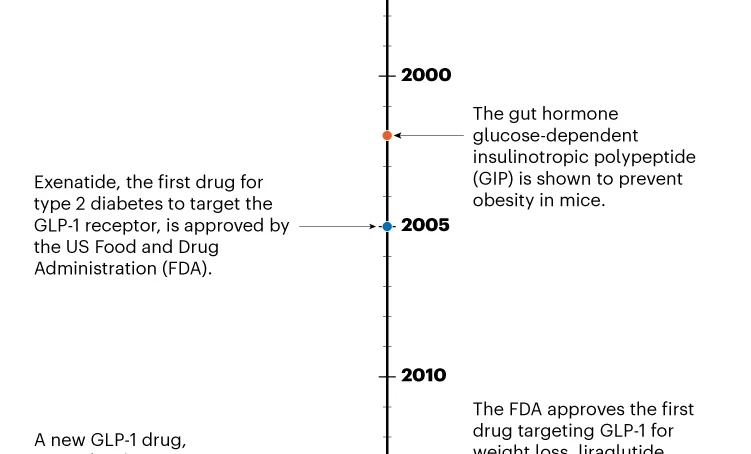
Tirzepatide doesn’t just target the GLP-1 receptor; it also mimics another hormone involved in insulin secretion, known as glucose-dependent insulinotropic polypeptide (GIP). Approved in 2022 for type 2 diabetes, this treatment – developed by Eli Lilly, based in Indianapolis, Indiana – led to a 21 per cent drop in body weight, on average, at the highest dose, compared with three per cent for placebo.
It’s unclear why mimicking both hormones works better than imitating just one. Müller says that tirzepatide might be a more potent activator of the GLP-1 receptor, and that GIP might help to make GLP-1’s side effects more tolerable, allowing for higher doses. It’s also possible that GIP might drive some weight loss on its own.
Despite the uncertainties, the levels of weight loss following tirzepatide treatment approach those typically achievable only through bariatric surgery. This procedure reduces body weight by 30 per cent or more after six months, and the weight loss continues for the next year or two.
“Ten years ago, if you had told me we have something that gets us pretty close [to bariatric surgery], I would have said that’s not possible,” says Ruth Gimeno, group vice-president of diabetes, obesity and cardiometabolic research and early clinical development at Eli Lilly.
The company plans to apply for the drug to be approved, pending results from a second phase III trial wrapping up in April 2023.
Despite tirzepatide’s promising results, it has researchers puzzled. It’s clear how GLP-1 helps to spur weight loss, but GIP’s role is a surprise. In fact, scientists have long thought that GIP actually encourages obesity: mice with dysfunctional GIP receptors are resistant to obesity.
Therefore, to induce weight loss, researchers thought the receptor should be switched off. But tirzepatide does the opposite.
“We were the first who came up with this crazy idea,” says Müller, who collaborates with Novo Nordisk. “And we were quite heavily criticized in the field.”
Müller and his colleagues – including DiMarchi and Tschöp – knew that GIP stimulates insulin secretion depending on blood glucose levels, just like GLP-1, says Müller. So, they developed molecules that mimicked both hormones.
After initial studies demonstrated that activating both the GIP and GLP-1 receptors caused weight loss, pharmaceutical companies created their own molecules achieving the same results, thus confirming that the method worked.
However, not everyone has changed their views on GIP. Holst feels that tirzepatide is simply a super powerful GLP-1 imitator.
It can also mimic GIP, “But it doesn’t really matter in patients with diabetes and obesity, because the GIP part doesn’t really do anything,” says Holst. Eli Lilly is conducting early-stage clinical trials with drugs that target GIP alone, which Holst says will resolve the ongoing debate.
And biopharmaceutical company Amgen, based in Thousand Oaks, California, is pursuing a drug that activates the GLP-1 receptor while thwarting the GIP receptor. Early clinical-trial data show that this treatment reduced body weight by up to around 15 per cent after 12 weeks.
Other approaches include ‘triple agonists’ that mimic the actions of GLP-1, GIP and a third hormone, glucagon, which also stimulates insulin secretion. Still other gut hormones involved in appetite, such as peptide YY, are being explored, too. And some researchers are investigating the monoclonal antibody bimagrumab, which increases muscle mass while decreasing fat.
One big question facing researchers now is whether people will need to take these medications for life to maintain their weight. A subset of clinical-trial participants who ceased taking semaglutide and stopped the study’s lifestyle interventions regained about two-thirds of their lost weight after one year.
Another unknown is who will respond to these drugs – and who won’t. It’s too early to tell now, but the drugs seem to be less effective for weight loss in people with type 2 diabetes than in those without. Conditions such as fatty liver disease and having fat around the organs, known as visceral body fat, might also affect how people respond to different drugs, Tschöp says.
Some researchers also worry that by offering a weight solution in societies that prize thinness, these drugs could also inadvertently reinforce the disputed link between excess weight and health. One study found that nearly 30 per cent of people who are considered obese are metabolically healthy.
Another showed that other health problems tend to be a better predictor of someone’s risk of death than is weight, demonstrating the need to consider factors other than weight when judging health, says Nutter.
“To pathologise a person’s health simply based on their body weight is potentially really, really harmful,” she adds.
Nutter is concerned that people might start these treatments – whose side effects, such as nausea and vomiting, can be severe – to escape weight stigma, rather than to serve a true health need.
Others worry about the idea that these drugs offer a quick fix. This is a common misconception about bariatric surgery, says Leslie Heinberg, a clinical psychologist at the Cleveland Clinic in Ohio who specialises in bariatric behavioural health and body image.
“Some people who still hold on to those mistaken beliefs will say, ‘Oh, now people can just take this pill and that’s the easy way out of obesity,’” she says.
Still, there is plenty of demand. And although these drugs are entering the market, not everyone who needs them will have access.
For a start, they are pricey – semaglutide for weight loss, branded as Wegovy, costs about $1,300 a month – and many insurance companies in the United States refuse to cover the expense, primarily owing to a misunderstanding of what causes obesity and viewing the treatments as ‘vanity drugs’.
“People talk about some of these drugs as being game-changers,” says Patty Nece, chair of the board of directors of the Obesity Action Coalition (OAC), an advocacy group based in Tampa, Florida. But, she adds, “For an individual patient, it’s never going to be a game-changer if they can’t afford it or don’t get access to it”.
Organisations such as the OAC are pushing pharmaceutical companies to offer affordability programmes. Eli Lilly, for example, has a ‘bridging programme’ for Mounjaro – tirzepatide for type 2 diabetes – under which the medication can cost as little as $25 for the first three months. Novo Nordisk has a similar programme for Wegovy.
Whatever the upfront costs, some scientists stress that addressing obesity could allow health-care systems to save enormous amounts of money by reducing a slew of conditions that are linked to the disease.
Although researchers are still chipping away at obesity’s complex combination of causes – including genetics, environment and behaviour – many support the idea that biology plays a significant part. Eating healthily and exercising will always be part of treatment, but many think that these drugs are a promising add-on.
Some researchers think that because these drugs act through biological mechanisms, they will help people to understand that a person’s body weight is often beyond their control through lifestyle changes alone. “Tirzepatide very clearly shows that it’s not about willpower,” Gimeno says.
- A Nature report











