All cells and tissues are constantly telling each other what they need and whether they’re stressed through molecular signalling.
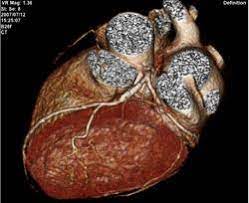
“When you lose a chunk of cells in a heart attack, you lose part of that conversation,” explains Charles Murry, an experimental pathologist and director of the Institute for Stem Cell and Regenerative Medicine at the University of Washington in Seattle.
Injected stem cells could be filling in the missing dialogue by secreting signalling and rescue molecules, he explains.
Although this sounds encouraging, there are still parts of the stem-cell-therapy approach that need to be finessed. In a 2018 study, Murry and colleagues transplanted approximately 750 million cardiomyocytes into macaque monkeys that had experienced major heart attacks.
One month after the intervention, the amount of blood pumped by their hearts had increased by 10.6 per cent compared with just 2.5 per cent in the control group. This advantage persisted three months later, but one out of the five stem-cell-treated monkeys suffered arrhythmias.
The onset of arrhythmia wasn’t previously observed in small-animal studies, but it is a known complication of heart attacks. Nevertheless, the researchers thought it could be a potential side effect of the stem-cell infusion.
“Obviously it isn’t statistically significant, but common sense led us to classify this as a treatment complication,” says Murry.
In addition to safety concerns, stem-cell therapies are also beset by questions of practicality. “Think of a lab with all these cell culture flasks where you have to grow millions of cells just to create a single dose,” says Terzic.
“Now imagine tens of thousands of patients. It’s a formidable effort to be ready, especially if you want to intervene rapidly. You don’t have the luxury of time to build up supplies.”
That’s one reason why some people think the promise of cardiac rejuvenation lies elsewhere. “There’s been an awful lot of time and money spent on stem-cell therapy, raising false hope in patients – and so far, the clinical outcomes have been largely disappointing,” says Paul Riley, a cardiovascular scientist at the University of Oxford, UK.
Riley is investigating whether inserting specific molecules into the heart might be more effective.
Human hearts can’t regenerate on their own, but other animals do have such abilities. Zebrafish, for example, can regrow their hearts after as much as 20 per cent is removed. New-born mice can also regenerate heart tissue.
Observing the molecular pathways in these animals might make similar results possible in humans.
Research has shown that following a myocardial infarction in zebrafish, the epicardium – a membrane surrounding the heart muscle – produces molecular signals that might kick-start muscle-cell regeneration. The hope is that manipulating the human epicardium could elicit the same therapeutic results.
“There are probably approaches we can take to target the cells that exist in the heart with small molecules or drugs, that could invoke repair and regeneration,” says Riley.
Back in 2011, Riley and colleagues showed that this is theoretically possible. They pre-treated adult mice with a daily injection of a protein called thymosin β4 for one week before inducing an infarction, and found that these mice were able to produce new cardiac muscle. This offers a road map to a pre-emptive therapy.
“If an individual is at high risk of a heart attack”, says Riley, “then it’s conceivable they could be advised to take a priming or preventative therapeutic, which may counteract an event, but it’s not quite the holy grail of restoring lost tissue after a heart attack that we’re searching for.”
In other studies, Riley has since shown that other proteins besides thymosin β4 might also have a role in stimulating the epicardium to regenerate the heart.
It’s easier to see how the drug route offers clearer prospects for scaling up – but the science behind this approach is newer, and there haven’t been any clinical trials in humans yet. “What goes in stem cells’ favour is the body of work behind them,” says Tehzeeb.
It might be that stem-cell therapies achieve government approvals first, but then drugs overtake them once the science and research have had time to catch up. “When we get to the end of the line with molecules, then maybe we can say stem cells are a thing of the past,” Tehzeeb says. “But until then, we should continue to pursue their potential.”
Murry echoes that sentiment, arguing that findings from both camps could end up helping everyone’s research. “We need an ecosystem with a competition of ideas, and as long as it’s all openly published then we’ll figure it out,” he says. “That’s the better approach, rather than saying my idea is better than your idea.”
- A Nature magazine report











