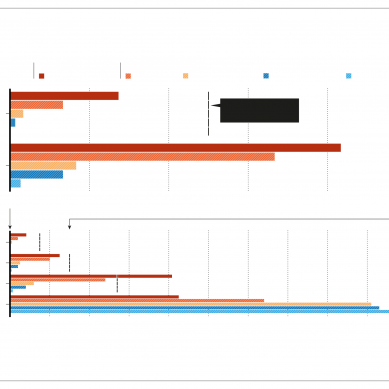
In Alabama in the united states, 37 per cent of counties are maternity care deserts – more than 240,000 women live in counties with no or little healthcare. About 39 per cent of counties don’t have a single obstetric provider.
Alabama is not alone in this. More than 2.2 million American women of childbearing age live in maternity care deserts, and another 4.8 million such women reside in counties with limited access to maternity care.
Angelica Lyons said she wanted to seek maternal care at another hospital but the University of Alabama was the only one near her home equipped to handle her high-risk pregnancy, which included high blood pressure near the beginning.
Dr Scott Harris, Alabama’s Department of Public Health State Health Officer, acknowledged the lack of access to care is a barrier for Black women who live in the state’s rural areas. Much of the state’s public health efforts are targeted along the rural Black Belt, which gets its name from the rich soil but it was also a region where many plantations were clustered.
Centuries later, the Black Belt continues to be a high-poverty region with a large Black population. More than half of the nation’s Black population lives in the South.
“We’ve talked a lot about structural racism and the impact of that on African American women and how it has no place in society,” Harris said. “I think we have to publicly call it what it is.”
She was eventually diagnosed with an excessive vomiting disorder, hyperemesis gravidarum, and was extremely dehydrated. Ansonia spent months in and out of the same hospital where her sister had been treated.
“They said, ‘Welcome to the pregnancy, sweetheart. This is what pregnancy is,’” Ansonia, 30, recalled. “I told her, ‘No, this is not normal for me to be throwing up 10 to 20 times a day.’ My own primary care wasn’t listening to me.”
Ansonia said throughout her pregnancy she encountered hospital staff that made stereotypical jokes, calling her child’s father her “baby daddy,” a trope often lobbed at Black parents.
“She said, ‘So, your baby daddy, where does he work?’” Ansonia recalled. “I said, ‘I don’t know what a baby daddy is but the father of my child is at work.’ She asked where he worked and I told her he had two businesses and she acted like she was surprised.”
Ansonia said staff assumed she didn’t have any health insurance, when she had insurance through her employer.
Ansonia has Type 2 diabetes and had issues with her blood pressure and heart throughout the pregnancy. She started to see a cardiologist and by the time she was 21 weeks pregnant, she was diagnosed with congestive heart failure. She was placed on a medley of medications, and her doctors decided to deliver the baby early via C-section.
Ansonia was scared, given everything she witnessed her sister go through nearly two years prior.
“There were several times I told my boyfriend that I thought that I was going to die,” she said.
Caesarean delivery rates are higher for Black women than white women, 36.8 per cent and 31 per cent, respectively, in 2021.
Problems continued for Ansonia after the delivery. She ended up needing a blood transfusion and was unable to see her son for his first few days of life.
A few months postpartum, she was still vomiting and having fainting spells that led to her being admitted to the hospital off and on. Her arms suffered from bruising from needles used to treat her throughout the pregnancy. She had always been slow to heal from any bruising, a common problem for diabetics.
Yet a doctor who had been involved throughout her entire pregnancy questioned why she had bruises on her arms and asked if she “smoked weed” or took any other recreational drugs. The hospital declined to comment, citing patient privacy laws.
“I said, ‘This is from me being stuck so many times and having to be in the hospital.’ I told him I don’t do any drugs,” she said.
He still sent her blood work off to be tested. The tests came back negative.
“That just made me not trust them, it made me not want to go back,” she said.
There are indications that the sufferings of Black mothers and their babies are being recognised, however late.
In 2019, US Representative Lauren Underwood, an Illinois Democrat, and Representative Alma Adams, a North Carolina Democrat, launched the Black Maternal Health Caucus. It is now one of the largest bipartisan congressional caucuses. The caucus introduced the Black Maternal Health Momnibus Act in 2019 and again in 2021, proposing sweeping changes that would increase funding and strengthen oversight. Key parts of the legislation have been adopted but the bill itself has yet to be approved.
Biden’s budget for fiscal year 2024 includes $471 million in funding to reduce maternal mortality and morbidity rates, expand maternal health initiatives in rural communities, and implicit bias training and other initiatives. It also requires states to provide continuous Medicaid coverage for 12 months postpartum, to eliminate gaps in health insurance. It also includes $1.9 billion in funding for women and child health programs.
US Secretary of Health and Human Services Xavier Becerra says more must be done at all levels of government to root out racism and bias within health care.
“We know that if we provide access to care for mother and baby for a full year, that we probably help produce not just good health results, but a promising future for mom and baby moving forward,” he said.
Shelonda Lyons always taught both her daughters the bitter truth of racism, hoping it would prepare them to navigate life growing up in Birmingham, the Deep South city known for its place in civil rights history.
“When we were young, she was showing us those images of all the Black people being hung, being burned on the trees,” Angelica said, pointing to a book that remains on the family’s coffee table. “She wanted us to understand it, to know where we lived and that racism was something that we might have to deal with.”
But Shelonda never could have prepared for the treatment her daughters endured during their pregnancies. She remembers feeling helpless and angry.
“It’s like a slap in the face to me because at what point do you realise that you’re dealing with human beings? That it doesn’t matter what colour they are,” she said, adding that now she worries any time they or her grandsons need to go to the doctor. “I don’t have a lot of trust.”
Angelica underwent two surgeries in the weeks that followed her C-section to repair internal damage and address her infection. She had to wear a colostomy bag for several months until she healed.
More than three years later, her stomach remains disfigured.
- An AP report