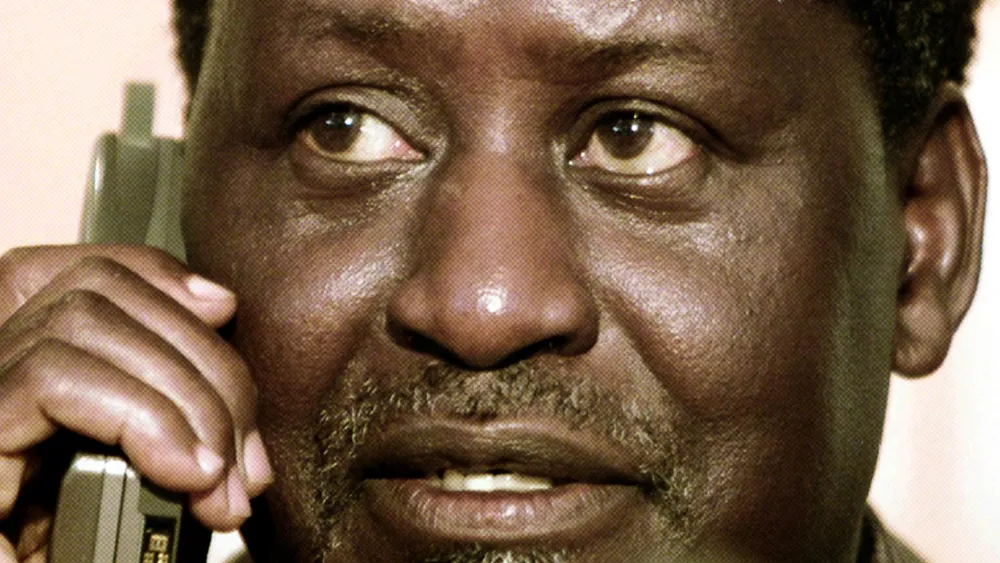
By the time Kevin Okal turned 47, life as he knew it had changed forever.
“I do not have saliva and cannot take dry foods anymore,” he says quietly, his voice steady but reflective. “I had to learn to live with it,” Okal opens up.
In 2019, Okal, a resident of Manyatta Estate in Kisumu City, began noticing strange symptoms, occasional nosebleeds, viscous sputum mixed with blood, and a blocked left ear, which he initially blamed on his weight. At the time, he weighed 105 kilogrammes.
However, a CT scan revealed a more alarming truth, a tumour in his maxillofacial region. He was referred to Ear, Nose and Throat (ENT) specialist David Odeng, who recommended a biopsy – a procedure where tissue samples are examined under a microscope to confirm the presence of disease.
“I underwent surgery to remove the tumour and the biopsy was done in July 2019,” Okal recalls.
The anxious wait for results was prolonged by a nationwide doctors’ and lab technicians’ strike. After two months, his worst fears were confirmed, Stage II Nasopharyngeal Carcinoma (NPC), a rare form of throat cancer that affects the upper part of the throat behind the nose and near the base of the skull.
Subsequent tests at other hospitals confirmed the diagnosis. Fortunately, the cancer had not spread to lymph nodes or other organs, giving him hope.
“I was told my chances of survival were high. That gave me the strength to fight on,” he says.
Scientists note that the disease becomes more dangerous when it spreads to nearby lymph nodes or distant organs.
Okal began treatment at Kenyatta National Hospital (KNH) in November 2019. Over the following months, he endured 33 chemotherapy sessions and five radiotherapy sessions.
The treatments came with severe side-effects – loss of taste, weight loss, swallowing difficulties, fatigue and cognitive fogginess that disrupted his personal and professional life.
“The experience was excruciating but I had to push through,” he says, adding that family support was vital during the ordeal.
“My mouth got dry, I had bruises and swallowing became painful. My eyes were so dry that I started seeing double,” he recalls.
These effects forced major changes to his relationship with food. Foods he once enjoyed became nearly impossible to eat. Today, he relies mostly on soups, smoothies, juices, and plenty of water between meals.
“If I eat ugali, I must take it with a lot of soup and water after every bite,” he says.
Despite these challenges, Okal never gave up. He credits his recovery to early diagnosis, discipline and adherence to medical advice.
He urges cancer patients to follow their doctors’ instructions faithfully, emphasising that side effects are part of the healing journey. “Some side effects fade quickly; others take longer. But they are manageable,” he assures.
Although not a habitual smoker, Okal admits that in his younger years, he would occasionally light a cigarette at social gatherings. “I would occasionally light up a cigarette at a party in my 30s,” he admits.
His experience underscores the risks posed not only by smoking but also by exposure to second-hand smoke. According to the World Health Organization (WHO) Global Status Report on Non-Communicable Diseases (NCDs) 2025, tobacco use and exposure to tobacco smoke are major risk factors for NCDs.
Research confirms that tobacco causes at least 16 types of cancer, including those of the lung, mouth, throat, oesophagus, stomach, pancreas, bladder, kidney, liver, cervix and nasopharynx, among others.
The Kenya Tobacco Control Data Initiative (TCDI) reports that 46 per cent of patients battling chronic illnesses such as cancer, cardiovascular disease and diabetes have a history of tobacco use. Tobacco smoking claims approximately 12,000 Kenyan lives annually, with 8.5 per cent of adults aged 15-65 using tobacco products.
Globally, nasopharyngeal cancer ranks 23rd among the most common cancers. In 2022, more than 120,000 new cases were reported worldwide, with Africa, South Asia and the Middle East bearing a disproportionate burden.
Dr Victor Oria, Chief Scientist at the Integrated Cancer Research Foundation of Kenya, explains that smoking exposes individuals to over 7,000 toxic chemicals, including at least 70 known carcinogens.
“These chemicals damage DNA and interfere with the body’s ability to repair itself, paving the way for mutations that cause cancer,” Dr Oria says. “Each puff introduces materials that can alter your DNA. Over time, these mutations accumulate, leading to cancer.”
He adds that tobacco smoke contains carcinogens that destroy the cells lining the mouth and throat. “Sometimes the carcinogenic chemicals in tobacco inhibit the cell’s ability to repair damaged DNA. When this continues over time, the accumulation of damage results in cancer,” Dr Oria elaborates.
Beyond personal suffering, the growing burden of NCDs, including cancer, is straining Kenya’s healthcare system. WHO projects that by 2030, NCD-related deaths will account for 55 percent of all deaths in the country.
Despite this looming crisis, Kenya’s health financing remains low, at around 3 per cent of GDP, far below the recommended 15 per cent under the Abuja Declaration.
Patrick Nyangweso, CEO of the National Taxpayers Association, argues that raising taxes on tobacco and nicotine products could help finance cancer treatment and prevention programmes.
“The tax collected from tobacco should directly fund cancer treatment and support survivors through the Emergency, Chronic and Critical Illness Fund,” he says.
Nyangweso suggests that policymakers should increase tobacco taxes to at least 70 per cent of retail price or 75 per cent of total taxes, in line with WHO recommendations. He points out that international evidence supports this approach.
“Countries that have consistently raised excise duty on tobacco have seen a sharp decline in smoking rates, especially among youth and low-income earners,” he explains.
France, for instance, has successfully reduced cigarette consumption by consistently increasing taxes, pushing the price of a packet to over Ksh1, 650 (€11).
For Okal, survival came with a renewed mission, to advocate for cancer screening, awareness and stronger tobacco control measures.
“This awareness must reach schools, hospitals, prisons, and workplaces,” he emphasises. “Many people still believe cancer is witchcraft. They only seek help when it’s too late.”
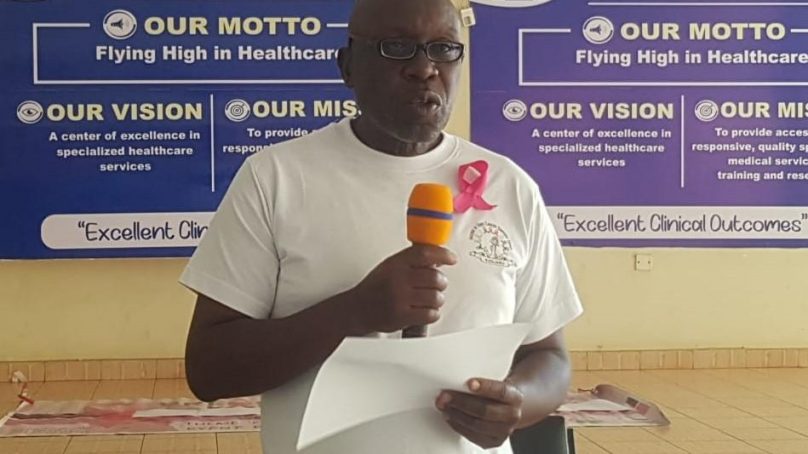
Today, the 53-year-old father of three works as a patient navigator at the Anchor of Hope Cancer Support Group at Jaramogi Oginga Odinga Teaching and Referral Hospital (JOOTRH) in Kisumu.
He helps patients navigate treatment procedures, offers emotional support and educates communities on early cancer screening and prevention. Okal, now cancer-free, continues to undergo annual medical reviews. His story of resilience and advocacy stands as a beacon of hope for others battling the disease.
“Cancer taught me that life is fragile, but it is worth fighting for,” he says, smiling. “I am alive today because I chose hope, followed treatment, and had people who stood by me.”
- A Tell Mdia / KNA report / By Robert Ojwang’