The fight against HIV in Kenya has received a major boost following the approval of Lenacapavir – a long-acting injectable HIV prevention drug.
Kenya is among the first nine African countries, set to introduce Lenacapavir by early January 2026, after WHO approved the twice-yearly jab as a highly effective method in curbing new HIV infections.
Lenacapavir received approval from the US Food and Drug Administration (FDA) in June 2025 and has been subsequently endorsed in the updated World Health Organisation (WHO) guidelines on long-acting HIV prevention, released in July 2025.
Lenacapavir is a twice-yearly injectable form of Pre-exposure Prophylaxis (PrEP) and it will complement existing PrEP options like taking daily pills and providing additional choices to meet diverse needs. It is designed to be discrete and convenient and also helps fight stigma.
The National HIV prevalence stands at 3.7 per cent, with 1.4 million people living with HIV, and a disquieting 41 per cent of new infections among youth under 24 years hence the urgency for impactful and tailored solutions has never been greater.
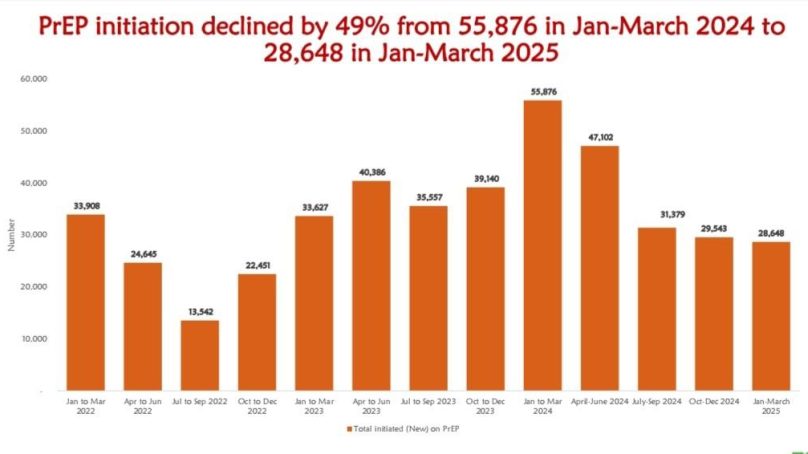
According to data from Kenya Health Information System, which shows Kenya has seen a sharp decline, in PrEP initiation of about 49 percent in a period of one year.
PrEP initiation refers to the process of starting someone on medication to prevent HIV infection before they are exposed to the virus. This typically involves assessing an individual’s risk factors, confirming they are HIV-negative and then prescribing and educating them on the appropriate PrEP regimen.
Policy Lead LVCT Health, Patriciah Jeckonia, while speaking during a science café organised by Media for Environment, Science, Health and Agriculture (Mesha) in a Nairobi hotel, said that the data revealed PreP initiation in the country declined by 49 per cent from 55,876 in January-March 2024 to 28, 648 in January – March 2025 period.
“Looking at the numbers we had in the previous year, the quarter of January to March and what we have this year, January to March, we see a decline in PrEP initiation in the country,” she said.
She said that it is an issue of concern because last year the country still recorded about 16,735 new infections at a time when we had committed that by 2020 we would have less than 8,000 new infections.
“The numbers show that there is still a lot of work to be done, especially amongst adolescents and young people, mostly adolescent girls and young women and there are new technologies that have come on board,” she said.
Jeckonia said that the country is looking forward, because Kenya has been selected as one of the nine early adopter countries for the roll out of the Lenacapavir drug adding that with a two-yearly injection, every six months, one is properly covered when it comes to HIV prevention needs.
She observed that the HIV landscape in Kenya, given the major funding cuts from donors, it is critical that stakeholders come together and have a discussion on what our HIV response should look like.
“I request the government to increase the domestic resource allocation, let us have the private sector come to the table with us, and let us figure out what the solution is. Let us also not leave behind the voices of communities,” she said.
Jeckonia noted that the funding decline in the country is a blow to the HIV response adding that we need to look more internally on how we can resource the HIV response domestically from the government.
“We know that a number of them are costly but also as a country we have to take stock of our priorities and really ensure that we can close the tap for new HIV infections,” she said.
Meanwhile, she said that data from Kenya Health Information System also showed that compared to the January-March 2025 to the same period the previous year, HIV testing declined by 38 per cent from 2,072,922 in Jan-March 2024 to 1,285,560 in January-March 2025.
HIV positivity increased from 1.2 per cent to 2.2 per cent in the same period. Females aged above 10 years accounted for 76 per cent of all HIV tests conducted between January-March 2025.
She observed that since we have the funding cuts it has also impacted on the mental well-being of people and that there is a direct correlation between mental health and HIV response.
“If your mental status is not okay, you are likely to miss your appointments, or miss taking your medication, and it can affect your overall well-being,” she said.
She stated that Kenya is one of those countries that is recognised for our progress in providing services to key populations, and these are populations that are at a higher risk of getting HIV.
“Now, with the transition, where the country has to take responsibility for the response, we have to find ways of providing services that are responsive to key populations in the spirit of universal health coverage, leaving no one behind,” she said.
Jeckonia said that it is high time that we have more of a social and behaviour change approach, to how we do our messaging, communicating in a way that influences decision making for the people who need the service, but also ensuring that the surrounding communities are supportive to whoever wants to access the service.
Meanwhile, Cabinet Secretary for Health Aden Duale has said that the Ministry through NASCOP and partners are working to ensure that Lenacapavir is accessible to Kenyans by January next year
“The government is committed to ensuring equitable access, strengthening community engagement, and integrating Lenacapavir into our national policies to reach priority populations effectively,” Duale said in a Press Release from his office on Tuesday.
The CS said this milestone underscores the government’s collective determination to expand access to effective, discreet, and sustainable HIV prevention options across the region noting that it has developed an implementation plan to facilitate a smooth roll out of Lenacapavir.
A report from the Ministry of Health in 2024 showed that an estimated 1.378 million Kenyans are living with HIV, with 97 per cent receiving treatment through a robust network of treatment centres.
- A Tell Media / KNA report / By Anita Omwenga







